-
속보 서산영덕고속도로 30여 대 추돌 등 사고…4명 사망재생

-
오늘 아침 6시 10분쯤 서산영덕고속도로 남상주 나들목 근처에서 30중 추돌 사고나 모두 4명이 숨졌습니다. 이만수 기자, 자세한 내용 전해주시죠. [기자] 네, 사고가 난건 오늘 이른 아침인 여섯 시 10분쯤입니다. 서산영덕고속도로 남상주 나들목 근처에서30중 추돌 사고가 발생했습니다. 사고 현장 모습을 보고 계신데요. 화면은 당진영덕고속도로 남상주나들목 영덕 방향 71. 8km 부근이라고 합니다. 지금까지 모두 네명이 숨지 것으로 파악되고 있습니다. 현재까지도 사고 여파가 이어지고 있어서저희도 조금 전에 근처 CCTV를 확인해 보니까 영덕방향, 그리고 청주 방향 모두 통제되고있습니다. 사고가 난 지 세시간 가까이 지났는데아직까지 사고 현장이모두 수습되지 않고 있는 겁니다. 사망자나 중상자가 늘어날까 걱정입니다. 지금 화면으로 보시다시피 사고 규모가 꽤 컸던 것 같습니다. 지금 화면으로 보더라도 차량들이 꽉 막혀 있고요. 저희가 다시 확인해 봤을 때도 통제는 계속되고 있었습니다. 조금 더 구체적인 사고 상황을 설명드리면 조금 전에 보셨던 대형 화물차가 있었는데요. 먼저 영덕방향으로 달리던 9. 5톤 화물차가 지금 보시는 것처럼 이렇게 가드레일을 뚫고 추락했다고 합니다. 그래서 화물차에 탑승하고 있던 운전자 한 명이 숨졌고요. 반대편으로 지금 화면으로 보시는 모습은, 이곳은 청주 방향인데 청주 방향에서도 사고가 나서 승용차에 타고 있던 3명이 모두 숨진 것으로 확인됐습니다. 아직까지 사망자의 정확한 신원은 확인되지 않고 있습니다. 저희가 지금 자막으로 30여 대 추돌사고다, 이렇게 말씀을 드리고 있는데요. 이게 조금 전에 소방당국에 확인해 보니까 30중 추돌사고는 아니고요. 사고가 난 곳 근처의 도로 위에 살얼음 때문에 동시다발적으로 비슷한 곳 근처에서 여러 건의 사고가 발생했고요. 그 사고로 인한 피해 차량을 집계해 봤더니 약 30여 대 정도 된다, 이렇게 추정하고 있습니다. 그래서 소방당국과 경찰은 오늘 아침에 난 사고 그리고 사망자 4명이 발생한 사고는 도로 위 살얼음 그러니까 블랙아이스 때문이 아닌가 일단 조금 더 구체적인 조사가 필요하겠지만 지금까지는 그렇게 추정하고 있습니다. [앵커] 그러니까 지금 사고가 30중 추돌사고 이거 하나가 난 게 아니라는 말씀이시죠? [기자] 그렇습니다. 30중 추돌사고 한 개가 아니고요. 지금 화면으로 보시고 계신 장소가 서산영덕고속도로 남상주나들목 근처인데 이 일대 도로 위에 광범위하게 도로 위에 살얼음, 그러니까 블랙아이스가 만들어져 있었던 것 같고요. 지금 보시는 화물차 사고 그리고 반대편에 있었던 승용차 사고를 포함해서 동시다발적으로 여러 군데에서 사고가 발생한 것 같습니다. 그리고 그 사고로 인한 피해 차량들을 집계해 봤더니 30여 대 정도가 된다, 이렇게 지금 소방당국 그리고 경찰은 설명하고 있습니다. 그래서 지금까지 확인된 피해는 일단 지금 보시는 화물차 운전자 1명, 조금 전에 보셨던 승용차에 탑승하고 있던 승객 3명, 모두 4명이고요. 하지만 오늘 사고 피해 규모가 꽤 크기 때문에 인명피해가 늘어날 수도 있을 것 같고요. 이 부분에 대해서는 확인되는 대로 다시 전해 드리도록 하겠습니다. [앵커] 그러니까 영덕 방향으로 달리던 화물차가 가드레일을 뚫고 추락해서 1명이 숨졌고 반대 방향에서는 30여 대 차량이 지금 블랙아이스로 인해서 피해가 발생한 것으로 추정되고 있는데 두 사고의 연관성이 있는 겁니까? [기자] 소방당국, 경찰의 설명에 따르면 각각 독립된 사고로 보인다고 설명하고 있습니다. 조금 전에 앵커께서 반대편에는 30여 대 추돌사고라고 설명하셨는데. 그게 아니고 그러니까 지금 화물차 사고가 있죠. 그리고 반대편에서 승용차 사고가 발생했습니다. 그리고 그 일대 고속도로 위에 넓게 곳곳에 블랙아이스가 만들어져 있었던 것 같고요. 그 근처에서 동시다발적으로 여러 사고가 발생한 것으로 보입니다. 그리고 피해 차량을 집계해 봤더니 30여 대 정도가 되는 것으로 보인다. 이렇게 소방과 경찰은 설명하고 있습니다. 물론 사고가 난 지 3시간 정도지만 아직까지 수습이 다 되고 있지 않기 때문에 사고 원인 그리고 30여 중 추돌사고인지 또 제가 설명드린 대로 여러 곳에서 동시다발적으로 사고가 나서 그 피해 차량이 30여 대 정도인지는 물론 조금 더 정확한 확인이 필요하긴 합니다. [앵커] 앞서서 블랙아이스가 원인으로 소방당국은 추정하고 있다라고 얘기를 해 주셨는데 지금 사고가 난 지역의 기온이 영하권인가요? 어떤 상황일까요? [기자] 사고가 난 지역의 정확한 날씨에 대해서 구체적인 정보를 가지고 있지는 않습니다. 다만 조금 전에 최승훈 기자도 포천 지역에서 전해 드렸다시피 오늘 경기 동북부 그리고 강원도 내륙 지방에 많은 눈이 예보되어 있었는데 저도 오늘 나오면서 확인해 보니까 서울 그리고 포천지역도 영상의 날씨라고 합니다. 그러니까 아마 이른 새벽에 눈 대신에 비가 내렸던 걸로 추정할 수 있을 것 같고요. 그 비가 내린 가운데 기온이 낮은 지역이 있었을 수 있지 않겠습니까? 그러면서 도로 위에 미세한 살얼음이 형성되지 않았나. 그래서 그로 인한 블랙아이스 형성으로 차량이 미끄러지면서 사고가 발생했을 가능성을 지금으로서는 염두에 두고서, 확정은 아니고요. 염두에 두고서 소방과 경찰당국이 조사를 이어가고 있지 않나 이렇게 예상해 볼 수 있을 것 같습니다. 하지만 단서를 달아야 되는 것이 지금은 사고 원인이나 이 부분에 대한 조사보다는 사고 수습 그리고 지금 벌써 4명이 숨졌기 때문에 더 이상 더 큰 인명피해가 없도록 하기 위해서 부상자들이 만약에 있다면 신속히 옮겨야 할 테고요. 사고 수습에 먼저 더 중점을 두고 있는 것으로 보입니다. [앵커] 지금 CCTV 화면을 봤으면 좋겠는데요. 앞서서 봤을 때는 양방향이 청주 방향으로는 아예 이동을 못하고 지금 꽉 차 있는 상황이었고 영덕 방향으로는 차량의 이동이 아예 없었거든요. 그러니까 앞선 지점에서 이미 통제가 시작된 상황이었는데. 지금 상황을 보면 영덕 방향으로는 차량이 달리고 있거든요. 이쪽은 통행이 가능한 걸까요? [기자] 그렇습니다. 지금 나가고 있는 화면, 그리고 20~30분 전에 확인했던 화면과 비교해 보면 차이가 있죠. 지금 보다시피 청주 방향은 차량이 거의 움직이지 못하고 있습니다. 지금 이렇게 보면 조금씩 움직이고 있는 것 같긴 한데. 사실상 거의 움직이지 않고 있는 것 같고요. 영덕 방향으로는 차량 소통이 조금씩 재개되고 있는 것 같습니다. 그리고 취재기자 김대근 기자가 같이 근무 중인데 메모를 보니까 말씀드렸다시피 추돌사고 역시 청주 방향뿐만 아니라 영덕 방향에서도 다 발생했다고 합니다. 그러니까 추돌사고가 청주 방향, 영덕 방향 곳곳에서 발생했고요. 아마 근처에 말씀드린 대로 도로 위 살얼음, 블랙아이스가 조금 넓게 형성되어 있었던 것 같고 동시다발적으로 사고가 발생해서 모두 30여 대 정도 차량들이 피해를 보지 않았나 이렇게 예상해 볼 수 있을 것 같습니다. [앵커] 오늘 전국적으로 그렇고 각 지역별로 일부 지역은 많은 눈도 예상되어 있어서 걱정인데 전체적으로 30중 추돌이기 때문에 수습까지는 오래 걸리지 않을까, 그런 우려가 있습니다. 어떻습니까? [기자] 조금 전에 확인하셨는데 영덕 방향은 어느 정도 수습이 이루어지고 있는 것 같고요. 화면으로 볼 때 지금 화면은 사고 초기 모습 같습니다. 조금 전에 저희가 확인했던 모습과는 다른데, 청주 방향으로는 지금 보시는 것처럼 사고 수습이 더딘 것 같습니다. 그런데 교통통제보다도 가장 걱정되는 것은 인명피해가 없어야 한다는 부분입니다. 아마 차량 사고를 수습하면서 추가 인명피해가 있는지 여부도 동시에 확인하면서 사고수습이 진행되고 있는 것으로 추정해 볼 수 있을 것 같습니다. [앵커] 알겠습니다. 사고와 관련해서 추가적인 내용 들어오는 대로 다시 전해 주시기 바랍니다. 사회부 이만수 기자였습니다. ※ ’당신의 제보가 뉴스가 됩니다’ [카카오톡] YTN 검색해 채널 추가 [전화] 02-398-8585 [메일] social@ytn.co.kr
-
일 한일 정상회담…중일 갈등 속 실용외교 시험대재생
-
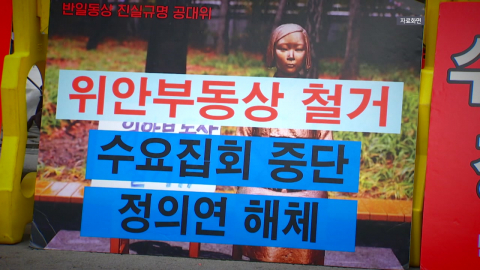
이재명 대통령이 오는 13일부터 1박 2일, 일본을 방문해 양국 정상 간 셔틀 외교를 이어갑니다. 중일 간 갈등이 고조되는 가운데 정부의 실용 외교가 다시 한 번 시험대에 오를 전망입니다. 김희준 기자입니다. [기자] 경주 APEC 정상회담에서 처음 대면한 지 두 달 반 만에 다시 만나는 이재명 대통령과 다카이치 사나에 일본 총리. 이번 무대는 다카이치 총리의 고향이자 지역구인 나라 현입니다. 두 정상은 북한 문제를 포함한 지역 및 국제 현안과 여러 민생 분야 협력 방안을 논의합니다. [위성락 /국가안보실장 : AI 등 미래 분야를 포함하여 스캠 등 초국가 범죄 대응, 사회 문제, 인적 교류 등 양국 간 민생에 직결된 분야에서 협력을 강화하기 위한 방안들이 폭넓게 논의될 것입니다] 최근 중국과 일본의 갈등이 고조되는 상황에서 한미일 안보협력 강화도 조율되는데, 현 정부 실용 외교가 다시 한 번 시험대에 오릅니다. 특히 중국의 대일 희토류 수출 통제 조치와 영향에 대한 대응도 거론될 것으로 보입니다. 앞서 한중 정상회담에서 시진핑 국가주석은 "역사의 올바른 편에 서라"며 사실상 일본을 겨냥해 한국을 우회 압박한 바 있습니다. [이재명 대통령(지난 7일) : 지금은 우리가 할 수 있는 게 매우 제한적으로 보여집니다. 나설 때 나서야지, 안 나설 때 나서면 별로 도움이 안 될 수도 있어요.] 과거사 문제와 관련해선 1942년 조세이 탄광 사고 조선인 유해 발굴 등 우선 인도적 측면에서 협력 계기를 만들겠다는 것이 정부 방침입니다. 이와 함께 일본이 주도하는 환태평양경제동반자 협정(CPTPP) 가입 등 다양한 경제 문제도 의제로 오릅니다. 이재명 정부 5번째 한일 정상회담. 셔틀 외교를 통해 미래지향적인 관계 발전의 토대를 더욱 확고히 하는 계기가 될지 주목됩니다. YTN 김희준입니다. ※ ’당신의 제보가 뉴스가 됩니다’ [카카오톡] YTN 검색해 채널 추가 [전화] 02-398-8585 [메일] social@ytn.co.kr












![[Y현장] "작품 속에 살아있을 이름"…'국민 배우' 안성기, 하늘의 별이 되다(종합)](https://image.ytn.co.kr/general/jpg/2026/0109/202601091042149519_h.jpg)
![[Y터뷰] '프로젝트 Y' 전종서 "한소희가 DM 보내 처음 알게 돼…답장했다"](https://image.ytn.co.kr/general/jpg/2026/0109/202601091441089698_h.jpg)

![[Y현장] 정우성, 고 안성기 추도사 "한국영화 온 마음으로 품은 선배님…영면하시길"](https://image.ytn.co.kr/general/jpg/2026/0109/202601091008157730_h.jpg)